ASSESSMENT SCALES
There are many different scales used to assess Degenerative Cervical Myelopathy (DCM), as we outline below. Myelopathy.org with AO Spine RECODE-DCM has defined the four that should be used as a minimum standard for future research studies, also known as a ‘core measurement set’, but they are not without limitations.
When conducting research, it is important to think carefully about the tools you wish to employ, to ensure those tools align with your research question, do not overly burden participants, incorporate the minimum standards for DCM, and also are reliable.
COSMIN or Consensus-based Standards for the Selection of Health Measurement Instruments is an international initiative that aims to support this decision-making. They have developed a framework to assess the evidence behind scales. We have applied this to DCM scales, and make this available below.
Some of the other key points to understand about assessments are:
When conducting research, it is important to think carefully about the tools you wish to employ, to ensure those tools align with your research question, do not overly burden participants, incorporate the minimum standards for DCM, and also are reliable.
COSMIN or Consensus-based Standards for the Selection of Health Measurement Instruments is an international initiative that aims to support this decision-making. They have developed a framework to assess the evidence behind scales. We have applied this to DCM scales, and make this available below.
Some of the other key points to understand about assessments are:
1) Not All Tools Are Designed to Measure the Same Aspect of DCM
Some tools measure just a single aspect of DCM, whilst others measure multiple aspects. Some tools have been specifically designed for use in DCM, whilst others have been repurposed from other areas of health.
2) Interpreting These Tools Can Be Complicated
No tool is perfect: All tools have their positives and negatives; for example, they may compromise on the detail and subtlety of measurements, to be shorter and easier to complete. All of these factors have a role in their accuracy and utility.
Be mindful of the numbers: most of these scoring systems use categories developed by researchers, which are then assigned a number. We are used to understanding numbers as a linear scale, i.e. 1 + 1 = 2, i.e. 2 is twice as big as 1. However, in the scoring systems, numbers and categories do not necessarily equate in this simple linear way. Therefore, a change in number or category could mean a very small change or a very large change in DCM.
Be mindful of the numbers: most of these scoring systems use categories developed by researchers, which are then assigned a number. We are used to understanding numbers as a linear scale, i.e. 1 + 1 = 2, i.e. 2 is twice as big as 1. However, in the scoring systems, numbers and categories do not necessarily equate in this simple linear way. Therefore, a change in number or category could mean a very small change or a very large change in DCM.
3) Scoring Systems Are Principally Used for Research but Are Increasingly Used in Routine Practice
Scoring systems are most commonly used in research studies, to objectively and accurately track changes in symptoms over time, perhaps in response to treatment. However, they are increasingly being used in normal routine care for the same reasons. The international guidelines for DCM [1] make use of the mJOA (modified Japanese Orthopaedic Association) score to help guide treatment decision-making.
The Modified Japanese Orthopaedic Association (mJOA) Scoring System
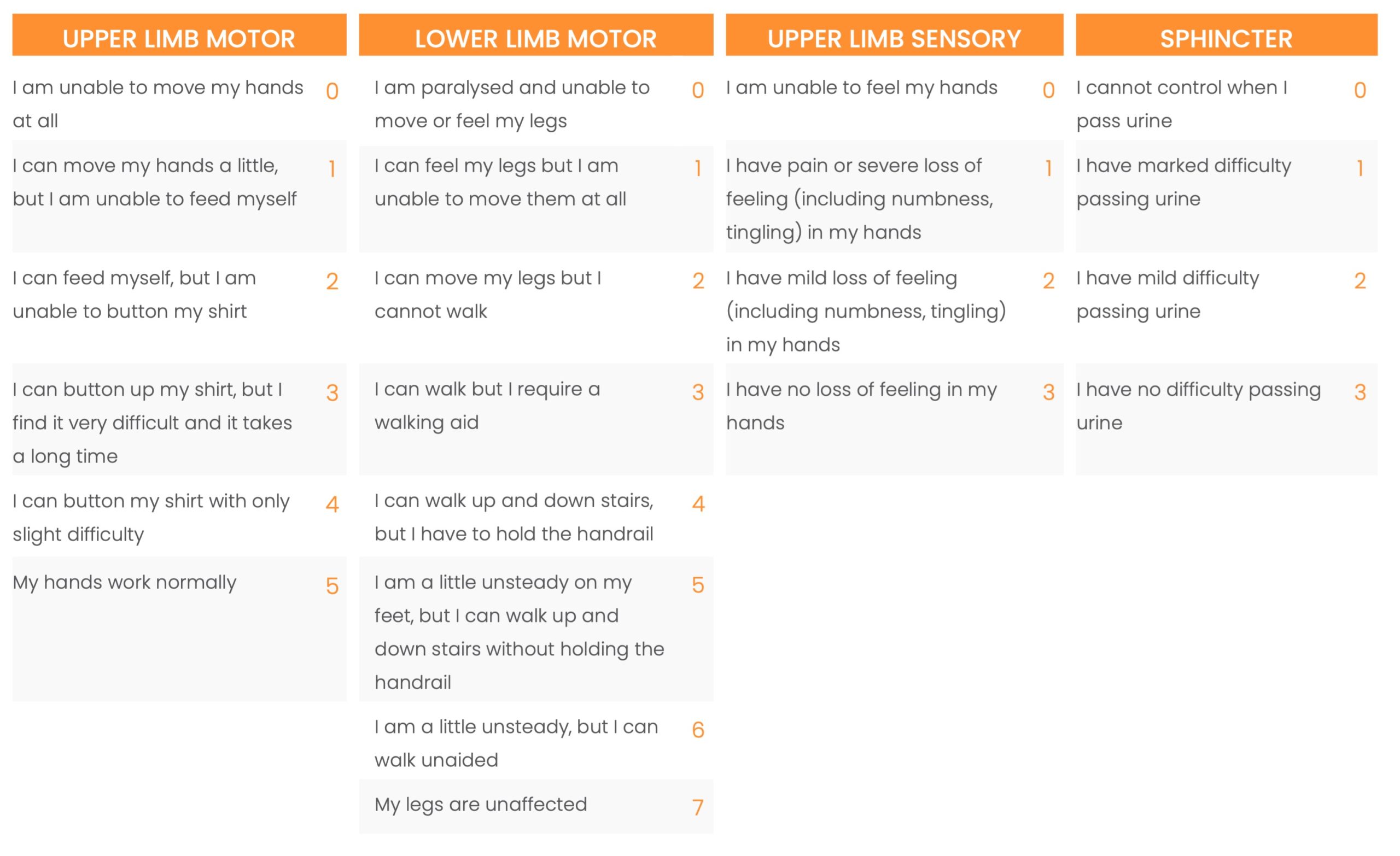
The mJOA scoring system is scored from 0 to 18 points. A lower score represents more severe DCM than a higher score. A score of 15–17 represents mild, 12–14 moderate, and 0–11 severe DCM. The mJOA comprises four parts: movement in the arms, movement in the legs, feeling in the arms, and bladder control, as shown below. Questions focus on everyday examples of how your DCM may be affecting you, such as how well you can button your shirt, feed yourself, walk, feel using your hands, and control your bladder.
The mJOA is used in the international guidelines for the management of DCM [1]. Doctors use the scoring system to grade the severity of DCM and advise on the best treatment strategy, which will normally be either watchful waiting with/without physiotherapy, or surgery.
4) Some Tools Are Completed by Professionals, and Others by People Living with DCM
Many scoring systems are simply completed by the doctor (Clinician Reported Outcome Measures or ClinROMs), based on the general information you provide during your consultation. Others require answers to very specific questions. Some tools are instead completed by the patient (Patient Reported Outcome Measures or PROMs). The time taken to complete the assessment will vary but may range between 2 and 45 minutes. It is important to consider this when introducing assessments to research studies, as long assessments are associated with participant attrition.
Below is a list of all of the assessment scales used in DCM research. We have listed them under the Core Outcome Set domains used by the AO Spine RECODE-DCM group.
You can click on a scale to see a synopsis of the tool, its quality rating, and the associated evidence.
Please note that, in many instances, the quality of the tool is considered low simply because studies have not yet evaluated its quality, rather than because studies have shown it to be a low-quality tool.
Improving assessments for DCM is recognised as a Top Research Priority by the AO Spine RECODE-DCM group.
Below is a list of all of the assessment scales used in DCM research. We have listed them under the Core Outcome Set domains used by the AO Spine RECODE-DCM group.
You can click on a scale to see a synopsis of the tool, its quality rating, and the associated evidence.
Please note that, in many instances, the quality of the tool is considered low simply because studies have not yet evaluated its quality, rather than because studies have shown it to be a low-quality tool.
Improving assessments for DCM is recognised as a Top Research Priority by the AO Spine RECODE-DCM group.
Neuromuscular Function
10-S Step Test
30MWT
9-Hole Peg Test
BBS
European Myelopathy Scale
Foot Tapping Test
Grip-And-Release Test
JOA
JOACMEQ
MDI
mJOA
Nurick Scale
P-mJOA
Ranawat Classification of Disease Severity
Triangle Step Test
30MWT
9-Hole Peg Test
BBS
European Myelopathy Scale
Foot Tapping Test
Grip-And-Release Test
JOA
JOACMEQ
MDI
mJOA
Nurick Scale
P-mJOA
Ranawat Classification of Disease Severity
Triangle Step Test
Life Impact
Pain
Adverse Events
No tools yet evaluated for use in DCM
Radiology
Cobb’s Method
CT (Tsuyama’s Classification, 2D & 3D)
CT (Tsuyama’s Classification, Lateral + Axial)
Ishihara’s Cervical Curvature Index
MRI (Depiction of Intramedullary Hyperintensity at Eight Cervical Disc Levels, T2W, 1.5-T or 3-T)
MRI (Kang’s Classification, 1.5-T or 3-T)
MRI (Muhle’s Classification, 1.5-T)
MRI (Vaccaro’s Classification, 1.5-T)
X-Rays (Computer-Assisted Measurement of Length & Thickness)
CT (Tsuyama’s Classification, 2D & 3D)
CT (Tsuyama’s Classification, Lateral + Axial)
Ishihara’s Cervical Curvature Index
MRI (Depiction of Intramedullary Hyperintensity at Eight Cervical Disc Levels, T2W, 1.5-T or 3-T)
MRI (Kang’s Classification, 1.5-T or 3-T)
MRI (Muhle’s Classification, 1.5-T)
MRI (Vaccaro’s Classification, 1.5-T)
X-Rays (Computer-Assisted Measurement of Length & Thickness)
Health Economics
No tools yet evaluated for use in DCM
